KOODAC
Meet KOODAC, whose aim is to develop orally bioavailable drugs that will dramatically improve cure rates for children affected by these cancers.
Team KOODAC is addressing the solid tumours in children challenge, to develop more effective, tailored therapies. In its latest study published in Cell, the team uncovered how the MYC oncoprotein helps tumours evade immune detection. Led by KOODAC co-lead Martin Eilers (University of Würzburg), the work highlights routes to targeting the oncogenic functions of MYC while leaving its physiological functions intact. Here, we talk to Martin and the first authors Leonie Uhl, Amel Aziba and Sinah Löbbert about the findings, which could finally enable successful immune therapies for solid tumours.
Through Cancer Grand Challenges team KOODAC is funded by Cancer Research UK, the French National Cancer Institute (INCa) and KiKa (Children Cancer Free Foundation).
Amel: The major aim of the Eilers lab is to understand how MYC oncoproteins drive tumourigenesis and by which mechanisms.
Martin: Previously it was always thought that the major oncogenic function of MYC was through transcriptional changes in gene expression and many things are well explained by that, for example MYC’s effects on metabolism. But there were always these lingering doubts. We've learned over the last decade that the major function of MYC in many tumours is to hide them from the immune system. But there was simply no mechanistic model to explain this.
Leonie: Here, we found that MYC is an RNA binding protein. We could map RNA binding to six amino acids, which we could then mutate without interfering with DNA binding to investigate MYC’s different functions.
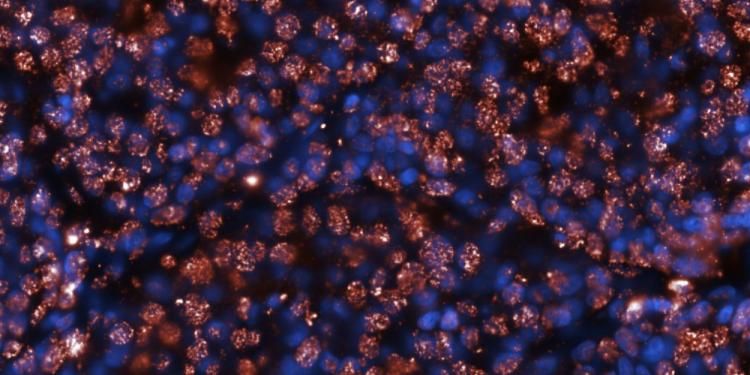
Through careful mechanistic experiments we put forward a model whereby in unperturbed conditions, MYC and MAX bind together to DNA and RNA polymerase is happily transcribing. However, if we induce RNA Pol 2 stalling and R-loop formation, we see redistribution of MYC away from its core promoter sites towards RNA. This transition promotes the formation of MYC condensates that concentrate and recruit RNA processing factors, getting rid of aberrantly accumulating RNA. If MYC is not there or deficient in RNA binding, this leads to the leakage of those RNAs into the cytosol where they would then activate innate immune signalling via binding to TLR-3.
Using the separation of function mutant, we investigated the importance of RNA binding in tumourigenesis in immunocompetent mice. In tumours where endogenous MYC has been knocked down, we could see that induction of the RNA binding mutant causes tumour regression, whereas wild-type MYC causes tumour growth.
Martin: In a nutshell, we found that RNA binding of MYC mediates immune evasion in pancreatic carcinoma. This provides a mechanistic model for how MYC mediates immune evasion, but it also changes the way we think about targeting MYC. The field has been looking for a way to somehow target its oncogenic function but leave physiological functions intact. I think this provides the route to do just that.
Sinah: Based on our findings in pancreatic cancer, we plan to explore strategies that target MYC RNA binding or that interfere with condensation, towards enhancing immune surveillance of tumours.
Martin: We're still working on this, but we have very strong evidence that MYC RNA binding is conserved for MYCN, which is a specific target for team KOODAC as a driver of childhood solid tumours. Nurix is very optimistic that DNA-encoded library (DEL) screening could identify compounds capable of disrupting this RNA binding complex.
Martin: We collaborated with Seychelle Voss (MIT) who is an exceptional structural biologist. Her lab successfully reconstituted the MYC–NEXT RNA processing complex from recombinant proteins, a remarkable achievement that now provides a tractable platform for Nurix team members to pursue drug discovery.
Martin: Our patient advocates are fabulous people and are deeply involved in the team’s work. One of the things we do is ask a patient advocate to tell the story of a researcher and a researcher to tell the story of a child. As a German academic it’s something I wasn’t used to, it's very emotional. It's a unique experience, which is intense but has a very strong impact.
Martin: KOODAC is simply the most exciting thing I've done in my life. It also turns out to be the most intense thing in my life, because Nurix brings to the table an absolutely industry style of doing things. So that has its own challenges, but it's incredibly exciting. This is the first collaboration I’ve been a part of which really works like clockwork, in the sense that all the different components really go hand in hand. The speed of progress is incredible.
Martin: Our findings provide a clear mechanistic explanation for how MYC suppresses innate immune activation in solid tumour models. Immune-based therapies have historically struggled in solid tumours, in part because tumour cells actively avoid immune detection. By identifying MYC as a central regulator of this process, we open the possibility that targeting MYC’s RNA binding function could help sensitise tumours to immunotherapy. If this mechanism is druggable, it will enable immune therapies for solid tumours, including those affecting children.
Through Cancer Grand Challenges team KOODAC is funded by Cancer Research UK, the French National Cancer Institute (INCa) and KiKa (Children Cancer Free Foundation).
Meet KOODAC, whose aim is to develop orally bioavailable drugs that will dramatically improve cure rates for children affected by these cancers.
Tackling solid tumors in children is so urgent that we set it as a challenge in successive rounds and funded three teams over the two calls.